Introduction
Seldom can prevalence have been so paradoxically matched by incomprehension,
or ignorance embarrassed by accessibility as in piles, for the disease is both
common and easy to inspect, and yet unnecessary confusion exists. There are two
reasons: a legacy of misleading terms related in turn to a misconceived
pathological explanation, and an inadequacy of anatomic description. Thus
disarmed by a stylized and simplistic image of anal anatomy and disabled by both
erroneous terminology and time-honored myths, the qualifying doctor can be
excused an inaccurate mental picture of what is in essence a simple complaint.
Given a true picture of the morphology of the anal lining, however, with an
understanding of its pertinent microscopic features one can readily perceive
both what piles are, how they occur, and what they would look like, and be able
to predict and envisage the complications to which they are prone.
The names 'haemorrhoids' and 'piles' are essentially synonymous though
differently derived from the two main—and only certain—symptoms, respectively
bleeding and protrusion. The disease, though, is not the result of varicosity
nor, as the reader will appreciate, are itching and pain its necessarily
expected accompaniments. All this, and their logical management, will become
clear from the anatomic account.
Anatomy of the anal lining
The anal canal is usually shown as a 4-cm long tube lined in its upper
two-thirds by insensible mucosa and below by a hairless, glandless cuff of
highly sensitive squamous epithelium, the anoderm. The mucosa is seen to be
thrown into longitudinal folds (named after Morgagni) which are
sometimes—incorrectly—depicted as containing vertically ascending columns of
serpigious veins. This oversimplified description derives from the usual method
of preservation and dissection and provides no clue either to the intricacies of
its infrastructure or the almost inevitable vagaries of its existence .
If, instead, the vessels of a fresh anorectum are filled (retrogradely, from
the superior rectal vein) prior to inflation and fixation, the interior of the
anal canal is seen, on transection of the rectum above, to look quite different . Now the anal lining
bulges into the lumen as three (occasionally four) pads—each more or less
impressed by the vertical mucosal folds—which have been called the anal
cushions. Their presence and curious architecture are the key to piles.
The anal cushions
Nineteenth-century anatomists gave a more accurate and detailed description
of the anal lining. One feature they recognized was the thickness and rich
vascularity of the anal submucosa. It was in fact likened to cavernous tissue
and reckoned to assist anal closure. The observation of its discontinuous
grouping into three main and constantly sited masses, however, explained the
nature of piles. We called them the anal cushions. There is often a fourth
midline posterior one and their substance extends above and below the dentate
line. When their component vasculature is filled they confer an appearance to
the anal lining which belies the standard anodyne description .
Blood supply
The anal cushions receive a rich intercommunicating supply from the superior,
middle, and inferior rectal (synonymously called haemorrhoidal) arteries. From
five to eight branches of the superior rectal artery pass from the mesorectum through muscular 'button
holes' in the rectal ampullary wall to descend into the anal submucosa , there to anastomose freely
with contributions from the middle and inferior vessels. Local mucosal
excisional procedures will inevitably encounter substantial bleeding from any
one or all three sources. Part of this supply is carried straight into the
venous system by direct arteriovenous shunts and probably provides for the
mechanical function (described below) without which the wealth of vasculature is
not fully explained.
The veins of the anal submucosa are particularly notable, exhibiting one of
the two entirely unique local morphological characteristics. They are
distinguished by discrete dilations along their course, particularly
subanodermally. These vein sacs, resemclover root, were once thought to be
pathological, and in fact the underlying fault in piles. John Hunter (1728–1793)
described them in a haemorrhoidectomy specimen (Spec. 1277, Hunterian Museum,
Royal College of Surgeons of England) and noted the great curiosity of their
being separated by segments of normal vein . They are, however, normal. They
occur in all adults and are found at birth . The subanodermal sacs look like
petals of a blue daisy through the skin of a baby's distracted anal verge, and
can also be demonstrated in the adult . They drain mainly cephalad into
the portal system but also through the sphincter and below it into the systemic
circulation; a route, though, that dissections suggest becomes increasingly
tenuous with age , which might explain the
postdefaecatory anal verge engorgement and oedema that troubles some patients,
and the oedema and discomfort of some prolapsed piles.
Support
The cushions are held against the shearing, extruding force of defaecation by
smooth muscle, the musculus submucosae ani, and by elastic tissue. This muscle,
the second unique anatomic feature—nowhere else is muscle to be found in the
submucosa—was discovered by Treitz (1853) and has been observed and drawn by
others since. It descends from the internal sphincter in separate bundles which coalesce subanodermally
to form a dense supporting stroma around the vein sacs . A longitudinal section shows its full extent and demonstrates how the looser
upper part of the cushions is supported by the tough more strongly secured lower
component, and how the muscle's contraction, which occurs during defaecation,
both flattens the cushions and braces them against the internal sphincter.
Function
There can be no doubt that the anal cushions contribute to anal closure. The
spongy substance and variable volume conferred by the vein sacs, with their
direct arterial communications, imparts an appropriate texture—firm, too, below
and floppy above—upon which the sphincter can 'squeeze' to complete closure. Of
interest, an inner tube of an inflated tyre falls naturally into three parts if
a band around its perimeter is tightened (David Tibbs, John Radcliffe
Hospital—personal communication).
The nature of piles
The anal cushions can as we have seen be viewed from above in an
appropriately prepared specimen . They can also be seen
anoscopically , in transverse histological section (, and by holding the dissected-free anal lining
up to the light . By whatever means of demonstration they are found
constantly to occupy the left lateral (3 o'clock), right posterior (7 o'clock),
and right anterior (11 o'clock) sectors of the anal circumference, and not
infrequently the posterior midline, which of course is where piles present. It
is logical to conclude, therefore, that the condition we call piles or
haemorrhoids results from the internal disruption and downward displacement of
the anal cushions, a conclusion supported by both their macroscopic and microscopic appearance . Varicosity of the anal veins, when it (rarely)
occurs, looks quite different.
Pathology
The anal cushions are disrupted to produce piles by the forces of
defaecation. For many sufferers defaecatory habits and stool consistency are
probably to blame. The Valsava effect of excessive straining engorges the
cushions, which have lost the support of the external sphincter as it relaxes.
The shearing force of hard stools will increase the damage. In other patients
who claim a lifetime of regular easy bowel actions, the anal cushions may be
structurally deficient. Weakness arising from the influence of progesterone on
smooth muscle and elastic tissue may explain the predisposition to haemorrhoids
in pregnancy, though an increase in pelvic vascularity may contribute. Many
women date their haemorrhoids not to actual pregnancy but to parturition, when
the supporting tissues of the anal cushions may be stretched and torn.
Histological examination often shows larger vascular spaces than normal and
more prominent connective tissues but no changes not accounted for by the
effects of disruption.
Classification
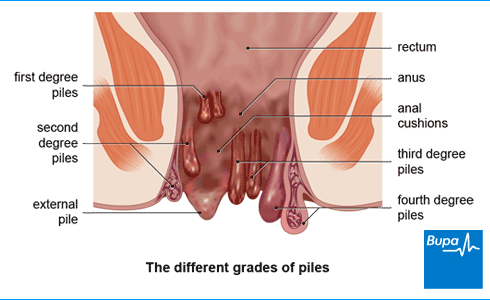
It is customary to classify haemorrhoids by degree: first degree, only
bleeding announces their presence; second degree, spontaneously reducing
prolapse at defaecation; third degree, prolapse requiring manual replacement;
fourth degree, permanent prolapse. However, while a classification is required
for the purpose of comparing different treatment techniques scientifically, the
degree of any particular patient's piles may in fact vary with time.
The terms 'internal' and 'external' piles add little.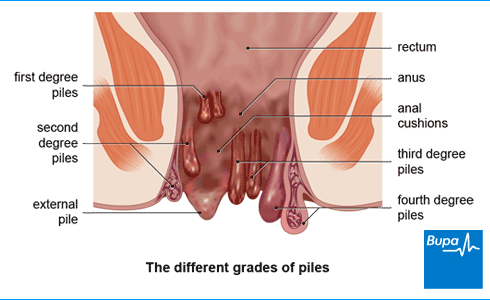
Symptoms
Although the underlying lesion in piles—disruption of the supporting and
anchoring tissues of the cushions—means that prolapse is inherent in their
nature, bleeding is more worrying and is the usual reason for seeing a doctor.
Prolapse is, however, the other unequivocal symptom. Pain, itching, and anal
dysfunctional effects are less reliable diagnostic criteria.
Bleeding
The capillaries of the lamina propria are only protected by a single layer of
epithelial cells, and little trauma is required to breach them. Since it is the
more lax-textured, upper part of the anal cushion which mainly prolapses,
dragging the mucosa to the outside, trauma due to wiping or contact with clothes
often occurs. Repeated trauma produces a chronic inflammatory response, making
the damaged mucosa a brighter red, and granular and so more friable and likely to bleed.
A great deal of unnecessary investigation, which is costly, inconvenient,
uncomfortable, and occasionally even hazardous for the patient, can be avoided
by time spent unravelling exactly what is meant by bleeding. Patient and
courteous attention to detail in taking a history is always amply repaid, but
never more so than here: haemorrhoids are very common, and yet bleeding may also
indicate a more serious condition. First- and second-degree piles, which remain
intra-anal except at defaecation, bleed with the bowel movement. Being capillary
blood it is bright red. If enquiry reveals that it occasionally drips, an anal
origin is certain, because the anus remains closed by tonic contraction of the
sphincter except at the moment of defaecation. Blood that drips into the pan,
after passage of the stool, must originate either from extruded anal mucosa, or
from a fissure in the anoderm. The only other, and most uncommon, possibility is
a rectal polyp on a long enough stalk. Similarly, bleeding into clothing is
almost certainly of anal origin. Blood smeared on the stool in the pan is
ominous and unlikely to be coming from piles, since freshly shed blood ought to
disperse into the water. The fact that it remains on the stool suggests either
that it has congealed there, or is mixed with mucus, indicating a higher
lesion.
Passage of clotted blood also demands exculpation of a colorectal source, and
a careful history may provide a useful clue. Piles may still be the explanation
if questioning reveals that the clots were only seen on the paper; such clotting
can have occurred in freshly shed blood lying at the anal verge. It is very rare
for a large pile to bleed back into the rectum and proclaim itself by passage of
older clots at stool.
Prolapse
Many patients have not tried manual replacement of their piles after
defaecation, having been 'afraid to', and therefore put up with more discomfort
than they need. Others replace them promptly only to be demoralized and
inconvenienced by their messy extrusion on exertion later.
Pain
Pain is a contentious issue in pile symptomatology. Although claimed to be a
prominent and attributable problem, there seems to be no good reason why a
disrupted anal cushion should actually be painful. When trapped outside the
closed anus, distortion combined with oedema and congestion from lymphatic and
venous impairment may well cause discomfort. In many cases pain on defaecation
is due to an easily overlooked fissure. None the less, some patients do
experience relief from what they had thought of as pain from successful
treatment of their uncomplicated piles, and the wise clinician allows for some
hyperbole, perhaps, in description.
Episodes of painful irreducible swelling which last a week or so can be most
unpleasant. Often called 'strangulated' piles or an 'attack of the piles', they
are usually due to greater or lesser degrees of infarction resulting from
obstruction of venous drainage by thrombosis and consecutive clotting in the
sacculated venous plexus. Infarction is used here in its proper sense, denoting
an intravascular and interstitial 'stuffing with blood', and not in its common
contemporary misusage implying necrosis. Although necrosis would supervene if
circulatory impairment by venous blockage were sufficient, complete obstruction
of venous return is in fact very rare and the usual outcome is spontaneous
resolution as the clot shrinks and lyses and venous circulation is
restored.
Itching
When the patient's main concern is itching, piles are seldom to blame. A
local skin condition is usually responsible. Although treatment of coexisting
piles may procure relief, it is unwise to encourage a patient greatly bothered
by pruritus to believe that the answer is at hand. Mucus discharge from a
prolapsed pile, however, causes an alleviable irritation in some patients.
Anorectal dysfunction
Defaecatory derangement can be excited by disrupted anal cushions causing a
sensation of incomplete evacuation, particularly when further engorged by
fruitless straining. Of course a feeling of unsatisfied defaecation—tenesmus—may
have a more serious explanation.
Soiling
Blood and serum from the exposed inflamed mucosal part of a pile dries dark
on underclothing and may be thought fecal. Only very rarely, however, do third-
and fourth-degree haemorrhoids allow minor conduction of rectal contents to the
surface. Mucus may also exude from the exteriorized mucosa of piles and can be
the presenting symptom.
Examination
When a meticulous history suggests piles and the findings agree, examination
can be confined to the anorectum. The only equipment then required is
proctoscope (anoscope), rigid sigmoidoscope (rectoscope), light source, and
biopsy forceps. Many, however, would disagree and argue for routine adjunctive
fiber-optic inspection of the distal colon, at least in those over 40 years of
age for rectal bleeding, however described and whatever the anoscopic findings.
Some workers in this field indeed advocate full colonoscopy in patients aged 40
or over presenting with rectal bleeding even when bright red, on the basis of
the frequency of finding right-sided pathology in those of middle age and older,
but in the author's view theirs is more an argument—still unresolved—for
screening.---buasir.jpg)
---buasir.jpg)
Signs
There are several dynamic influences on a pile's presentation—the vigorous
arterial supply, the presence and possibly changing diameter of the
arteriovenous shunts, the variability of cushion bulk due to the capacity of the
venous saccules, and the effects of cushion displacement and anal sphincter
contraction on venous and lymphatic drainage. As a result, not only does the
appearance change from time to time in the same patient, but the same symptom
may have different causes. For instance, whereas most people complaining of
prolapse have simple displacement of the anal cushion(s) , a 'lump' felt by others may be
due to engorgement of the subanodermal veins from, one presumes, impaired
drainage or transient but most uncomfortable postdefaecatory
anodermal oedema. .
Piles that are transiently displaced suffer little trauma, but when the
mucosal part is frequently exposed it becomes inflamed . Thrombosis and clotting in the vein sacs also
influence the appearance of the pile, but as an indication there will be
associated discomfort or, depending on the extent of clotting and consequent
infarction, frank pain. Clotting of a small part of the venous plexus causes an
uncomfortable attack of swelling of the pile, with oedema but little infarction.
Greater degrees of obliteration of venous drainage embarrass the circulation
accordingly . However, even the fully infarcted pile will, despite its appearance, resolve. Many patients
who seek medical attention because of such an attack of saccular clotting, and
who graphically describe the severity of the condition, have recovered by the
time of specialist consultation. The term 'strangulated piles' may be misapplied
to this condition, causing inappropriate and inevitably unsuccessful efforts at
supposedly therapeutic replacement.
A disordered cushion may, therefore, present in one of several ways as a lump
at the anal verge. Commonly, however, external inspection provides no clue to
their presence, and nothing abnormal is found on anal digitation, since
uncomplicated piles are impalpable. A nodular induration is felt if clotting has
occurred. In most patients, the diagnosis is suggested by the history and
confirmed with the anoscope. Interpretation of the appearance is not
straightforward. Since anal cushions are normal structures , their distinction from piles is only one of degree. Bright red granularity of the
mucosal part of a cushion is certain evidence of its disruption, and the extent
to which the cushions bulge into the instrument's end on straining and follow it
out on withdrawal, provide a valuable guide. The beginner will often miss the
anoscopic diagnosis of piles from failing to ask the patient to push down as if
defaecating as the instrument is gradually withdrawn. A previously unimpressive
anal cushion may then demonstrate its obvious disruption.
Rectoscopic (rigid 'sigmoidoscopic') exclusion of rectal disease is an
essential part of the establishment of the diagnosis. Because piles are common,
finding them does not rule out another condition higher in the rectum causing
the symptoms. There is, however, no evidence for the claim still occasionally
made that haemorrhoids can result from rectal carcinoma or pelvic masses.
Differential diagnosis
Anal tags
Many patients mistake anal tags for piles, and indeed the disrupted anodermal
part of a cushion may have a similar appearance. Anal tags are cutaneous
protruberances at the junction of the anoderm and perianal skin. They are of
uncertain origin, but possibly result from local derangement of lymphatic
drainage—as their occasional disarming partial reformation soon after excision
suggests. They can be solitary and discrete, or form a circumferential irregular
fringe .
Fibroepithelial polyp
These are club-like protruberances from the dentate line and seem to be
hypertrophied anal papillas, again possibly due to lymphatic obstruction .
Sentinel pile
This misnomer is given to a skin tag marking—and often containing within
it—the distal end of an anal fissure, found usually in the posterior midline .
Fissure
A patient described as having 'painful itchy piles' may well be suffering
from an anal fissure, particularly when associated with a sentinel tag
masquerading as a pile. The deep burning pain of a fissure on and after
defaecation and the associated itching are quite unlike the discomfort
appropriate to a pile. Typically, too, the pain of a fissure will start some
30 min after defaecation and continue for 2 to several hours.
Dermatitis
Because of the widespread belief, both in the lay and the medical mind, that
itching and soreness mean piles, in many patients referred for a surgical
opinion the problem is in fact dermatological. Hyperkeratosis (seen as pale,
slightly soggy or glazed skin), erythema, punctate excoriations, and multiple
hairline radiating cracks—often more pronounced in the anterior or posterior
midlines—will suggest the correct diagnosis . While the occasional patient
may have psoriasis and quite a few are prone to itchy rashes elsewhere, in most,
in the author's experience, the problem is confined to the anus. The pain at
defaecation of anodermatitis usually lasts only a matter of seconds.
'Perianal haematoma'
The term 'pile' might easily have been inspired by this condition (Latin:
pila = ball) so spherical and usually singular is it , and its other name, 'thrombosed external
pile', is not entirely inappropriate. However, to keep our terminology exact we
should use 'pile' to denote a disrupted anal cushion. These often painful
lesions of sudden onset and, when not relieved by incision, of usually
self-limiting nature (either by rupture or by absorption) are not in fact the
ruptured blood vessel the term suggests (nor are they strictly speaking
'perianal', arising as they do subanodermally) but vein sacs distended by clot.
The term 'clotted vein sac' describes them accurately but though preferable is
unlikely to supersede its time-honoured alternative.
Rectal prolapse
Early rectal prolapse may be confused with piles when the patient is unable
to describe the size of the protrusion and is inhibited from straining
sufficiently at the examination to produce it. Treatment for piles may then be
instituted with later disappointment, but no substantial harm done.
Rectal tumour
Rectal tumour can easily be missed by impatient history taking and
unreflective digital examination, for it is not so much the length of the finger
which matters as the amount of thought behind it. Because of the rectum's
curvature, even upper-third tumours may be palpable. Even when nothing is felt
or seen, if the patient's symptoms do not accord with the findings further
investigation is required. Ominous symptoms are old blood, particularly if slimy
or clotted, tenesmus, altered bowel behaviour, deep discomfort, and
'wet'—messy—flatus.
Miscellaneous
It is a curious fact that almost any discomfort in or irregularity of the
anorectum may be attributed to piles. Thus proctalgia fugax, proctitis, solitary
rectal ulcer, fistula-in-ano, and warts may also all masquerade.
Treatment
Since piles may be blamed for almost any anal condition the first step is to
decide whether they could be responsible for the symptoms. When itching is the
main complaint piles are unlikely to be the cause, and actual pain—rather than
the discomfort of protrusion or episodes attributable to attacks of
thrombosis—is more likely to be due to a fissure. Chronic anal pain, of course,
is never due to piles. With prolapse and bleeding, however, we are on firmer
ground.
The management will be either conservative or interventional.
Conservative treatment
Although piles are by definition disrupted anal cushions, symptoms from them
are partly determined by their size, which can alter greatly depending on the
state of engorgement of their constituent vein sacs, which in turn is affected
by straining and the state of tone of the surrounding anal sphincter. Simple
avoidance of prolonged straining at stool may achieve sufficient symptomatic
relief. An increase in dietary fiber, therefore, and desistance from reading in
the lavatory, together with advice to ignore the false signal suggesting the
need for a greater straining effort imparted sometimes by prolapsing piles may
be enough.
Interventional treatment
Surgical measures work by reducing the bulk of the disrupted anal cushion
(not only has its attachment loosened but its internal structure as well), and
inducing adhesion of the remainder. Since the mucosal part causes most of the
symptoms—all of the bleeding and mucus discharge, and most of the discomfort—its
reduction will be sufficient for the majority of patients. Even a large
cutaneous component may be pulled up and so be flattened and tidied by tissue
reduction above. It is therefore fortunate that the mucosa is insensitive and so
allows quick and effective treatment in the outpatient clinic or office. Various
techniques are available.
Rubber band ligation
In 'banding', as it is called, a 'polyp' of the pile centred sufficiently
cephalad to prevent involvement of the sensitive anoderm is pulled into a
ligating device passed down the anoscope and strangulated by displacing from the
ring-mounting a small rubber O-ring previously rolled there from a cone loader.
The incorporated tissue withers and falls away within 2 or 3 days leaving a
small ulcer which is usually healed in a month.
The size of the 'polyp' banded will depend on the toughness of the tissue,
the volume of redundant loose cushion, and the traction force applied by the
operator. Previous intervention—banding, injection, and so on—may cause such
dense scarring as to prevent the incorporation of sufficient tissue to help.
Usually, however, with good grasping forceps a polyp the size of an average
raspberry can be banded, and sometimes, gratifyingly, the size of a large one.
Because the anatomy of the anal canal and the mechanics of banding make it
impossible to ablate enough tissue to be damaging, the author takes the view
that the greater the volume of the mucosal part of the pile which can be
ensnared the better. The pile is therefore first carefully 'sized up' down the
anoscope to choose the site to be seized by the graspers which will ensure the
strangulation of the greatest part of the pile without involving the anoderm. If
the amount of tissue obtained seems less than expected, a further application,
this time firmly grasping and pulling on the previously banded polyp, will often
achieve more . If on the other hand the band looks to have been
placed too high or too low, a further adjoining application is worthwhile .
Even permanently prolapsed irreducible piles can be cured by banding. The
band can be applied to the exposed mucosa outside the anal canal with complete
symptomatic relief, even the cutaneous/anodermal element being improved, and
anyway seldom much of a nuisance .
Several banding instrument models are available and although they work on the
same broad principle there are two main categories, single-operator and
assistant-required. As well as their self-evident attraction, single-operator
banders confer the advantage that in holding the proctoscope throughout the
surgeon can keep it exactly on the selected target. There are three types. One,
a suction device (which can be driven by the Venturi effect of a running tap),
uses a metal sucker tube—with the banding rubber ring mounted at its end and
displaceable by a trigger—to suck the pile to which it is applied (under vision
down any proctoscope) into it. Although straightforward to use, the need for
suction may create practical difficulties, and the impossibility of knowing how
much tissue has been sucked into the end for banding and how much suction can
safely be applied without causing avulsion are deterring factors. Another
consists simply of a small-diameter proctoscope with the rubber O-ring, again
displaceable by a releasing mechanism, mounted at the operating end. A
theoretical disadvantage to its use may be the problem of inadequacy of view.
The 'One-man bander' seems to overcome both these disadvantages . Several loaded ones are kept ready so that even
multiple banding can be the work of a moment. It is designed for use down the
Naunton-Morgan 'rectal speculum', a proctoscope, in fact, whose wide diameter
allows a more certain diagnosis of piles than those of smaller bore (which may
prevent their appreciation through providing too narrow a view). It is certainly
the author's experience that piles can easily be missed down narrow
anoscopes.
For grasping the pile, Irvin-Moore's nasal conchal forceps seem ideally
suited. They open more widely within the ring of the ligator than at least one
purpose-designed model, and grip the tissue with less danger of tearing .
On a note of caution, it has been the author's experience that combining pile
banding with an anal stretch procedure may precipitate clotting in the residual
sacculated venous plexus and so cause severe anal cushion infarction with its
associated pain and swelling.
An empty rectum making banding easier and certainly more agreeable if not
safer, it is best to have the patient self-administer a mini-enema or glycerin
suppository prior to the banding. In addition, in case any pain afterwards would
otherwise inhibit defaecation, it is sensible to advise patients to start a
week's course of ispaghula husk or similar the day before. Finally, to make the
procedure and its immediate aftermath as comfortable as possible the patients
are also given analgesic tablets to take an hour before, and a supply to use
afterwards.
Infrared photocoagulation and bipolar diathermy
Both of these cause tissue destruction by heat. The instruments are applied
through an anoscope to coagulate a predictable volume of adjoining tissue. The
mucosal part is treated so no anaesthesia is required.
In bipolar diathermy the mucosa is simply grasped by the instrument and the
intervening tissue destroyed by an electric current passed across from one
electrode to the other.
Sclerotherapy
An irritant chemical solution, usually 3 ml of 5 per cent phenol in arachis
oil, is injected into the submucosa of the mucosal part of each pile. When the
varicose vein theory of piles prevailed it was thought to act by inducing
fibrosis which constricted the superior rectal venous drainage, so, it was
thought, deterring the causative—as they thought (from the human's erect
posture)—transmission of the supposed high pressures from the portal system. In
fact it probably causes shrinkage of tissue by necrosis, and adhesion as a
result of the ensuing inflammatory reaction.
Cryotherapy
A liquid nitrogen probe is placed against the pile for 3 min, and causes cold
necrosis. Local anaesthesia, at least, is said to be needed.
Laser treatment
Laser evaporation has also been used for pile excision, with good initial
reports. Its theoretical attraction lies in the reduction to the minimum of
damage to residual tissue. However, it is an elaborate way of performing a
simple task and uses expensive and fallible equipment in a forgiving area of
great blood supply and margin for error in which excellent results can be
obtained by simpler means. Were it to prove significantly less painful than
scissor excision, and perhaps to allow more rapid healing, neither of which has
so far been shown, then it might find widespread use.
Haemorrhoidectomy
When the troublesome cutaneous part of a pile is too large or immobile for
patient relief simply from addressing the mucosal moiety above, scissor
excision—haemorrhoidectomy—is required. However, although not 'ambulant', it is
therapy that can often be done under local anaesthetic and seldom requires much
more than an overnight stay. The excessively painful and prolonged experience of
folk memory resulted mainly from the well intentioned use of wide-bore rubber
drains or packs inserted in theater against the risk of haemorrhage. Mistaken,
too, was the much encouraged belief that three-sector excision was always
required ('the operation's over when it looks like a clover'), a practice
unfounded in either trial or systematic experience. It arose with little doubt
from the appearance of even normal anal cushions after anal manipulation in the
lithotomy position, particularly when a patient is 'light' and strains under the
anaesthetic. In fact the surgeon should be guided by the disease and will
therefore sometimes excise in only one place, although in other cases in four.
Always, however, adequate bridges of healthy tissue must be left between
excision sites because not only is the anoderm of great functional importance in
continence—'sampling' the rectal contents before release—but its excessive
removal will result in a stricture, an avoidable tragedy. The other half of the
mnemonic is certainly true, 'if it looks like a dahlia it'll end up a
failure'.
The patient's rectum should be emptied prior to surgery by means of an enema
administered about 2 h before. Whereas in the United Kingdom the patient is
usually put 'in lithotomy' for the procedure, the prone jack-knife position is
probably preferable for reasons both of access and local conditions, the anal
canal's axis then being in a line with the surgeon's eye rather than, as in the
lithotomy position, at an angle to it, and the vasculature not being unnaturally
suffused with blood. However, the lithotomy position and the lateral position
with buttocks taped apart, also useful, are easier to arrange.
Haemorrhoidectomy can be performed either open or closed and is done with
scissors or diathermy (or for that matter, laser). Either way, the essential
principle, emphasized by the reminder that surgery is the replacement of one
lesion by another, is to keep the damage to the minimum required for symptomatic
relief. Remember, too, that piles are just overlarge, floppy, and displaced
parts of a structure which almost certainly contributes to anal control, so
excision should leave sufficient behind. Above all, ample 'bridges' should be
left. Finally, the midline anoderm, particularly posteriorly, being so unstable
and prone to fissure, it is as well to stay away from it. Therefore, a
symptomatic midline posterior pile, as can occur, may be better treated by band
ligation—so above the dentate line—with acceptance of any residual cutaneous
irregularity there.
Open—excision/ligation—haemorrhoidectomy was popularized by Milligan and his
colleagues at St Marks Hospital, London. Forceps are applied to the cutaneous
part of the pile at the anal verge to reveal the mucosal moiety. A second pair
then grasps the main pile mass which is thereby lifted from its surroundings. It
is then snipped from the adjoining skin in a racket-shaped cut whose wide
handle, directed cephalad above the dentate line, contains the superior rectal
contribution to its blood supply . The elliptical part of the cut overlying the
intersphincteric groove passes through the subanodermal part of the
haemorrhoidal venous plexus to reveal the discrete vein sacs within. It is
deepened to reveal the lower border of the internal sphincter. The pile is then
dissected from the internal sphincter for a few millimetres (emerging fibres of
Treitz's muscle will be encountered and divided)—both by identifying to
safeguard it and to allow ligation above the dentate line (so of insensitive
tissue)—so creating a thick pedicle which is transfixed and ligated . The ligated remnant—most is excised—falls away in
a few days to allow the open wound to heal by secondary intention. Despite that
much diathermy coagulation may be required at the edges to achieve haemostasis,
the wound usually contracts rapidly and will be found almost closed in as little
as 10 days.
The closed method, with or without submucosal excision of adjoining
'haemorrhoidal' tissue, was designed for faster healing and less pain. (The term
'haemorrhoidal' here illustrates the confusion which misleading terminology
engenders. The spongy cavernous-like submucosa of the anal canal serves a
valuable function in continence. Calling it 'haemorrhoidal' suggests disease and
so encourages excision). It has not, however, been shown to achieve either aim,
neither pain relief nor healing being improved. (Confoundingly,
haemorrhoidectomy was also no more comfortable after a smooth muscle relaxant or
internal sphincter division (lateral sphincterotomy)).
By operating down a wide-diameter slotted speculum the pile can be excised in
its anatomic position without distortion, a technique which recommends itself
from first principles alone. The pile exposed in the slot is excised within an
ellipse, exposing the internal sphincter in its base, narrow enough to allow
closure without tension . It is a technique which has been found most
satisfactory.
After haemorrhoidectomy by whichever method, light dressings are placed over
the anus, perhaps kept in place by elasticated pants for easy changing. If
general anaesthesia has been used the anal wounds should be thoroughly
infiltrated with a long-acting local anaesthetic. The anus should not be packed.
Warm baths are comforting, with or without salt, and measures are taken to keep
the stools soft and regular. There is no need for the patient to stay in
hospital until the bowels have moved but if they have not by the third day the
patient should report back for an enema. Antibiotic cover is not required unless
there is a particular predisposition to sepsis.
Manual anal dilation
This was widely practised as a treatment for piles in the last century. The
nineteenth-century French surgeon, Verneuil, again reconciling its effect with
the varicose vein theory, thought it improved venous drainage by stretching the
rectal muscular button holes which convey the anal tributaries of the superior
rectal vein. When reintroduced some years ago, it transiently displaced the
surgical standby of the time, haemorrhoidectomy, but was later shown to have
limited application. It probably helps patients who have discomfort and
difficulty in defaecation by easing the effort of evacuation, so reducing the
congestion of the cushions from excessive straining.
Pile stitching
This has been advocated. Absorbable sutures are placed above the dentate line
to attach the cushion back to the internal sphincter. Obliteration of its blood
supply also reduces bulk. It has a place when large piles demand amelioration
yet there is a substantial risk from haemorrhage—in the presence of a cavernous
haemangiomatous deformity, for instance, or when a patient must not discontinue
anticoagulants.
Complications
Ephemeral
Vasovagal
A few people—mainly young males in the author's experience—faint after
banding of piles, and even injection. It is therefore sensible to warn all
patients to arrange to be driven home.
Pain
Some discomfort follows all the tissue ablative procedures but amounts in
some patients to severe pain lasting as long as a week. Again, prior knowledge
will prevent much needless worry and also allow the patient to plan in
advance.
Haemorrhage
Tissue destructive or excisional techniques will also leave a well
vascularized, raw wet surface and so carry the irreducible risk of secondary
haemorrhage. It is rare, but when it occurs, alarming, but once more if the
patient is told of the possibility beforehand there will be less anxiety and
disruption. In the author's experience only once in 20 years has continued
bleeding required suture for haemostasis. In the other dozen or so instances the
bleeding stopped spontaneously and without resort even to attempted tamponade
with a balloon catheter. A micronized flavonidic fraction of diosmin and
hesperidin (Daflon) significantly reduced secondary haemorrhage in one trial,
and in an experience of 12 patients with secondary haemorrhage after
haemorrhoidectomy a submucosal injection of 1:10 000 epinephrine through a
proctoscope under sedation secured haemostasis each time.
Infection
Sepsis is an uncommon complication and will be treated on its merits. Fatal
sepsis even after simple banding has been reported in immunocompromised
patients. Stories are handed down of portal pyemia following haemorrhoidectomy,
and of necrotizing fasciitis complicating it. Both no doubt have occurred and
will again but must be excessively rare. Neat surgery with the least trauma will
surely reduce the possibility as will patient selection and judicious drainage
rather than skin closure when the tissues have been compromised.
Urinary
Haemorrhoidectomy is notorious for causing transient difficulty in voiding in
men. Banding may also induce curious bladder symptoms. Inadvertent intra- or
periprostatic injection of sclerosant may have serious sequelae, even impotence
being reported.
Anal cushion thrombosis
Occasionally, excessive pain seems to be attributable to thrombosis/clotting
in the residual anal cushion after pile banding, the complication being
detectable by the digital discovery of knobbly induration within the anal
canal.
Permanent
Impairment of continence
A thorough study of 172 patients who had undergone haemorrhoidectomy at least
3 years previously (at a time when three sector excision was standard) found
that 26 per cent had experienced a consequent impairment of control. Given the
function of the anal cushions and the fact that haemorrhoidectomy may have been
relegated to the end of the operating list to be performed by an unsupervised
trainee, this outcome is not greatly surprising. However, if the surgeon
confines tissue removal to the clearly redundant and leaves what Waldeyer called
the 'corpus cavernosum recti' substantially intact, no functional impairment
need be feared.
Oedema and tags
Occasionally, however careful the excision, the intervening skin bridges may
swell uncomfortably with oedema to remain afterwards as tags. Though lymphatic
impairment, perhaps from diathermy damage, is presumably responsible, the
aetiology of anal tags is obscure; furthermore, when the entire anal lining has
dislocated to form a circular curtain at the anus, the intervening bridges will
of necessity remain as tags. They can be improved later under local anaesthesia
if required.
Stricture
The anal lining is extraordinarily forgiving; elastic, robust, and quick
healing. Only inexcusably excessive excision will result in stenosis, or some
other extraordinary circumstance.
Which treatment?
A generation ago the choice was limited; for bleeding there was injection,
and for prolapse haemorrhoidectomy. Nowadays open surgery is seldom necessary.
The invention of outpatient tissue-reducing techniques has not only increased
the possibilities but improved the prospect. At the same time the introduction
of prospective randomized clinical trials has for the first time enabled
scientific evaluation.
Conservative treatment has been compared with band ligation; bulk purgatives
or high fibre diet with sclerotherapy, stretching, sphincterotomy, band
ligation, and freezing. Banding has also been compared with sclerotherapy,
haemorrhoidectomy, stretching, and infrared photocoagulation. Photocoagulation
has been compared with bipolar diathermy, and one type of haemorrhoidectomy has
been judged against another. Excellent and praiseworthy though such trials are
they suggest a 'rivalry', when in fact no one treatment is best for all
patients. Their greater merit is in showing prospectively and with careful
control and monitoring that benefit can be derived from each measure, so
allowing us an informed choice of the possible treatments.
However, while infrared- and electrocoagulation achieve the same objective
with less pain and time off work, band ligation requires significantly fewer
treatment sessions, and the instrument used is both cheaper and more robust.
Multiple banding having been shown to be no more painful than a single
application per visit, in the author's experience the great majority of patients
are put right at one attendance. A recent overview, in fact, concluded that
rubber-band ligation was the most effective 'ambulant' measure available.
Haemorrhoidectomy though requiring admission, anaesthesia, and a longer
recovery, still retains its place when the cutaneous part of the pile is causing
the problem. Careful and targeted surgery will be rewarded by an excellent
result and a most satisfied, relieved patient.
Cryodestruction is an anatomically less accurate means of tissue ablation and
leaves a smelly, weeping wound slow to heal. Laser surgery offers attractive
qualities but, given the rapidity of both doing and recovering from simple
scissor excision and the cost of the equipment required, it seems unlikely to be
preferred.
Manual anal dilation may have the occasional adjunctive place in the
management of piles but would no longer be advocated as primary treatment.
Management of infarcted ('strangulated') piles
When one reflects on the necessarily turbulent flow in the sacculated venous
plexus it seems odd how seldom thrombosis and clotting occurs. Afflicting a pile
it causes considerable swelling and discomfort, and invites attempts at
immediate amelioration. However, there have not been, and are unlikely ever to
be, randomized trials of conservative and surgical treatment. In the author's
experience the infarction is only rarely so dense as to cause insupportable pain
and lead to necrosis, so most patients can be reassured that natural
thrombolysis will restore the circulation and result in resolution in about
10 days . Nitroglycerin ointment is reported to provide
dramatic relief from the pain. In severe cases, however, there is no doubt that
debridement haemorrhoidectomy, excising the worse afflicted tissue, is rewarded
by rapid deliverance from misery .
For the majority sufficient relief will be obtained by rest, analgesics, and
hot baths, and by the medical attendant's confident prediction that the worst
will be over in a week or at the most 10 days. Meanwhile they will be best
advised to ensure soft regular stools by the daily consumption of ispaghula husk
or its alternatives.
Conclusion
Once one understands the detailed anatomy of haemorrhoids and their
pathological possibilities, their management is straightforward, and the
treatment effective, acceptable, and reasonably trouble free. The important part
is diagnosis. The patient's preconception that piles are responsible for their
symptoms must not cloud the clinician's mind, for it does not take long
experience in a busy anorectal disorder practice to realize that many patients
sailing under the pennant of piles have something functional, dermatological, or
otherwise idiopathic causing their symptoms. Uppermost must be the question
whether reducing the bulk of the anal cushions and mooring them more firmly will
logically address the presenting problem. If not, then in a nineteenth-century
surgeon's words, 'in such cases prudence equally forbids the rash interposition
of unavailing art, and the useless indulgence of delusive hope'.
After being in relationship with Wilson for seven years,he broke up with me, I did everything possible to bring him back but all was in vain, I wanted him back so much because of the love I have for him, I begged him with everything, I made promises but he refused. I explained my problem to someone online and she suggested that I should contact a spell caster that could help me cast a spell to bring him back but I am the type that don't believed in spell, I had no choice than to try it, I meant a spell caster called Dr Zuma zuk and I email him, and he told me there was no problem that everything will be okay before three days, that my ex will return to me before three days, he cast the spell and surprisingly in the second day, it was around 4pm. My ex called me, I was so surprised, I answered the call and all he said was that he was so sorry for everything that happened, that he wanted me to return to him, that he loves me so much. I was so happy and went to him, that was how we started living together happily again. Since then, I have made promise that anybody I know that have a relationship problem, I would be of help to such person by referring him or her to the only real and powerful spell caster who helped me with my own problem and who is different from all the fake ones out there. Anybody could need the help of the spell caster, his email: spiritualherbalisthealing@gmail.com or call him +2348164728160 you can email him if you need his assistance in your relationship or anything. CONTACT HIM NOW FOR SOLUTION TO ALL YOUR PROBLEMS
ReplyDelete